Schizophrenia Complete Guide: Symptoms, Causes and Recovery
Despite affecting 24 million people globally, 64% of Americans still believe schizophrenia means “split personality”—yet breakthrough 2024 treatments and recovery research prove 75% of people achieve significant improvement with proper support.
Key Takeaways:
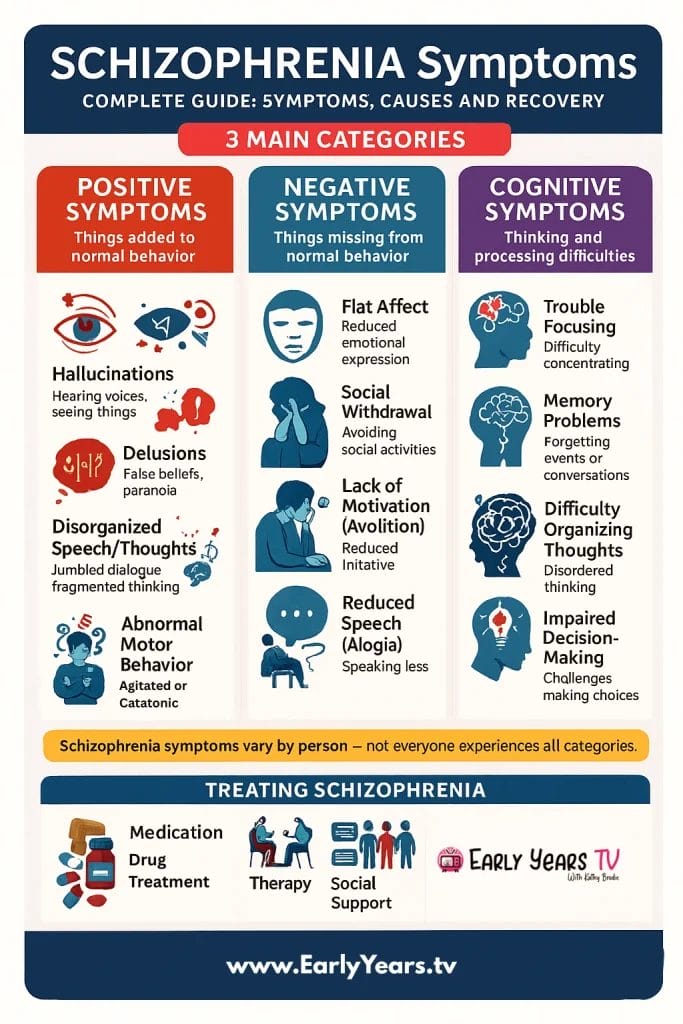
- What are the main symptoms of schizophrenia? Schizophrenia involves three symptom types: positive symptoms (hallucinations, delusions), negative symptoms (reduced motivation, emotional expression), and cognitive symptoms (memory, attention problems). Most people experience combinations of these symptoms, which respond differently to treatment approaches.
- Can people with schizophrenia recover? Yes—25% achieve complete recovery and 75% show significant improvement with proper treatment. Breakthrough 2024 medications like Cobenfy, coordinated specialty care programs, and early intervention within two years of symptom onset dramatically improve long-term outcomes and quality of life.
Introduction
Schizophrenia affects approximately 1% of the global population, yet despite decades of research and treatment advances, widespread misconceptions persist about this complex neurobiological condition. Far from the “split personality” myth popularized by media, schizophrenia is a treatable mental health condition characterized by altered perception, thought patterns, and emotional responses.
Current research brings hope: 25% of people with schizophrenia achieve complete recovery, while 50% experience significant improvement with appropriate treatment. Modern interventions, including breakthrough medications approved in 2024 and comprehensive psychosocial approaches, offer unprecedented opportunities for recovery and meaningful life engagement.
This comprehensive guide explores the real symptoms of schizophrenia, evidence-based causes, and most importantly, the pathways to recovery. Whether you’re experiencing concerning symptoms, supporting a loved one, or seeking accurate information, understanding schizophrenia through a recovery-focused lens can transform outcomes. Like other neurodivergent mental health conditions, schizophrenia requires specialized understanding and comprehensive support approaches that honor the person’s full experience and potential.
Medical Disclaimer: This guide provides educational information only and should not replace professional medical advice, diagnosis, or treatment. Always consult qualified healthcare providers for personalized care.
Understanding Schizophrenia: The Basics
Schizophrenia represents a neurobiological condition affecting how the brain processes information, emotions, and sensory experiences. Unlike popular misconceptions, people with schizophrenia maintain a single, continuous personality—the condition involves altered perception of reality rather than multiple identities.
The condition typically emerges during late adolescence and early adulthood, with peak onset occurring between ages 16-30 for men and 20-35 for women. This timing coincides with critical brain development periods, when the prefrontal cortex undergoes final maturation processes. Women often experience later onset and may show different symptom presentations, particularly around hormonal transitions like menopause.
Globally, schizophrenia affects approximately 24 million people, representing roughly 1 in 300 individuals worldwide. The condition occurs across all cultures, ethnicities, and socioeconomic backgrounds, though environmental factors can influence symptom expression and treatment access. Urban birth rates show 2-3 times higher incidence compared to rural areas, suggesting environmental influences on development.
Research consistently demonstrates that schizophrenia involves multiple brain networks rather than single brain abnormalities. Neuroimaging studies reveal differences in brain structure and connectivity, particularly in areas responsible for executive function, working memory, and sensory processing. These biological findings support understanding schizophrenia as a medical condition requiring comprehensive treatment approaches.
Common Myths vs. Reality
Addressing misconceptions about schizophrenia remains crucial for reducing stigma and promoting accurate understanding. Public education surveys reveal that 64% of Americans incorrectly believe schizophrenia involves “split personality,” while 32% associate the condition primarily with violence.
| Myth | Reality |
|---|---|
| Split personality disorder | Single personality with altered perception of reality |
| Always violent and dangerous | 90% are not violent; more likely to be victims of violence |
| Completely untreatable condition | 75% show significant improvement with comprehensive treatment |
| Caused by bad parenting or personal weakness | Neurobiological condition with genetic and environmental components |
| People cannot work or live independently | Many achieve employment, education, and independent living goals |
| Symptoms are constant and unchanging | Symptoms fluctuate; many people experience periods of stability |
These misconceptions contribute to discrimination in employment, housing, and healthcare settings. Family members often report that stigma impacts their loved ones more significantly than the symptoms themselves. Education and direct contact with people in recovery represent the most effective approaches for changing attitudes and promoting inclusion.
The Three Types of Schizophrenia Symptoms
Mental health professionals categorize schizophrenia symptoms into three primary groups: positive symptoms (additions to normal experience), negative symptoms (reductions in normal functioning), and cognitive symptoms (changes in thinking processes). Understanding these categories helps families and individuals recognize patterns and communicate effectively with healthcare providers.
Positive Symptoms: When Reality Becomes Distorted
Positive symptoms represent experiences that typically aren’t present in unaffected individuals. Despite the term “positive,” these symptoms often cause significant distress and require immediate clinical attention. These symptoms respond most readily to antipsychotic medications, with 70-80% of people experiencing substantial improvement.
Hallucinations affect approximately 70% of people with schizophrenia, with auditory hallucinations being most common. These voices may seem to come from outside the person’s head, often commenting on behavior, giving commands, or engaging in conversations. Visual hallucinations occur less frequently but can involve seeing people, objects, or lights that others cannot perceive. Tactile, olfactory, and gustatory hallucinations may also occur, though these are relatively rare.
Real-world examples include hearing voices criticizing daily activities (“You’re making breakfast wrong”), experiencing running commentary (“Now she’s walking to the store”), or perceiving elaborate conversations between multiple voices. Some people develop coping strategies like wearing headphones or engaging in activities that reduce hallucination frequency.
Delusions involve firmly held false beliefs that persist despite contradictory evidence. Persecutory delusions—beliefs that others are plotting harm—affect approximately 80% of people experiencing delusions. Grandiose delusions involve beliefs about having special powers, identity, or mission. Referential delusions include interpreting neutral events as personally meaningful, such as believing television programs contain special messages.
Examples include believing neighbors are monitoring activities through hidden cameras, thinking celebrities are communicating through song lyrics, or maintaining that family members have been replaced by imposters. These beliefs feel completely real to the person experiencing them and often influence behavior and decision-making.
Disorganized thinking and speech manifest as difficulty organizing thoughts logically or expressing ideas coherently. Speech may jump between topics without clear connections (derailment), include made-up words (neologisms), or become completely incomprehensible (word salad). Some people experience thought blocking, where ideas suddenly stop mid-sentence.
Disorganized or abnormal motor behavior ranges from childlike silliness to unpredictable agitation. Catatonic behaviors include maintaining unusual postures, excessive motor activity without purpose, or complete motionlessness. These symptoms significantly impact daily functioning and safety.
Negative Symptoms: When Abilities Diminish
Negative symptoms involve reductions in normal emotional, behavioral, and cognitive functioning. These symptoms often prove more challenging to treat than positive symptoms and significantly impact long-term functioning and quality of life. Approximately 40-50% of people experience meaningful improvement in negative symptoms with comprehensive treatment approaches.
Reduced emotional expression (flat affect) appears as decreased facial expressions, limited eye contact, and reduced vocal inflection. This doesn’t mean the person lacks emotions internally—rather, their ability to express emotions outwardly becomes impaired. Family members often misinterpret this as lack of caring or engagement, creating relationship strain.
Decreased motivation (avolition) affects the ability to initiate and sustain goal-directed activities. This differs from laziness or lack of interest—people often want to engage in activities but find themselves unable to begin or complete tasks. Simple activities like showering, cooking, or answering phone calls may become overwhelming challenges.
Social withdrawal (asociality) involves reduced interest in social interactions and relationships. People may stop contacting friends, avoid family gatherings, or feel uncomfortable in previously enjoyed social situations. This withdrawal often occurs gradually, making it difficult for others to recognize as a symptom rather than personal choice.
Reduced speech (alogia) manifests as brief, empty responses to questions or complete lack of spontaneous conversation. People may provide minimal information when asked direct questions and rarely initiate conversations. This symptom significantly impacts relationships and employment opportunities.
Decreased pleasure (anhedonia) involves reduced ability to experience joy, satisfaction, or pleasure from previously enjoyed activities. Hobbies, relationships, food, or entertainment may no longer provide positive feelings. This symptom often contributes to depression and social isolation.
Understanding how these symptoms develop helps families recognize that behavioral changes often reflect illness progression rather than personal choices. Effective treatment approaches address negative symptoms through medication adjustments, psychosocial interventions, and environmental modifications.
Cognitive Symptoms: The Hidden Impact
Cognitive symptoms affect thinking processes and often receive less attention than positive or negative symptoms, yet they significantly impact daily functioning and recovery outcomes. These symptoms may appear before other schizophrenia symptoms emerge and often persist even when positive symptoms improve with treatment.
Executive functioning difficulties involve problems with planning, organizing, and completing complex tasks. People may struggle with cooking multi-step meals, managing finances, or following medication schedules. These challenges often interfere with independent living goals and employment success.
Working memory problems affect the ability to hold and manipulate information mentally. This impacts following conversations, remembering instructions, or keeping track of multiple tasks simultaneously. Simple activities like grocery shopping become challenging when people cannot remember their list while navigating the store.
Attention and concentration issues manifest as difficulty focusing on tasks, easy distractibility, or inability to filter out irrelevant information. Reading, watching movies, or participating in lengthy conversations may become exhausting. These symptoms significantly impact educational and occupational functioning.
Processing speed reduction involves slower thinking and responding compared to previous functioning levels. People may need additional time to understand questions, formulate responses, or complete tasks. This doesn’t reflect intelligence changes but rather altered information processing efficiency.
Real-world examples include struggling to follow recipe instructions while cooking, losing track of conversations in noisy environments, or needing multiple attempts to complete work assignments previously managed easily. These symptoms often frustrate individuals who recognize their capabilities have changed.
| Symptom Type | Daily Life Impact | Treatment Response |
|---|---|---|
| Positive | Acute distress, crisis situations requiring immediate intervention | 70-80% respond well to antipsychotic medication |
| Negative | Long-term functioning challenges, relationship difficulties | 40-50% improvement with comprehensive treatment approaches |
| Cognitive | Work/school performance, independent living skills | 30-40% improvement with cognitive training and environmental supports |
Cognitive rehabilitation programs, including computerized training and skills coaching, show promise for improving these symptoms. Environmental modifications like reducing distractions, providing written instructions, and breaking complex tasks into smaller steps help people manage cognitive challenges effectively.
Early Warning Signs and When to Seek Help
Recognizing early signs of schizophrenia enables timely intervention, which significantly improves long-term outcomes. Research demonstrates that people receiving treatment within the first two years of symptom onset show better recovery rates, reduced hospitalization needs, and maintained functioning in education and employment.
Prodromal Phase: The Early Indicators
The prodromal phase represents the period before full psychotic symptoms emerge, often lasting months to years. During this time, subtle changes in thinking, behavior, and functioning may signal developing illness. Family members and friends often notice these changes before the individual recognizes them as concerning.
Social withdrawal and isolation frequently represent the first noticeable changes. People may gradually reduce contact with friends, skip social activities they previously enjoyed, or spend increasing time alone in their rooms. This withdrawal differs from typical adolescent independence-seeking and often feels concerning to family members.
Decline in academic or work performance occurs despite previous competence and effort. Grades may drop, work quality decreases, or people may struggle with tasks they previously managed easily. Teachers, employers, or supervisors may express concerns about changed performance levels.
Unusual thoughts or suspicions emerge gradually, often involving increased paranoia about others’ intentions or beliefs that ordinary events hold special meaning. People may become convinced that classmates are talking about them, neighbors are watching their activities, or random events contain personal messages.
Changes in sleep patterns include difficulty falling asleep, frequent awakening, or complete sleep schedule disruption. Some people experience vivid, disturbing dreams or report feeling unrested despite adequate sleep hours. These changes often precede other symptoms by weeks or months.
Decreased personal hygiene and self-care involves neglecting previously maintained grooming standards, wearing the same clothes repeatedly, or showing reduced concern about personal appearance. This change typically feels unusual for the individual’s established patterns.
Family education about prodromal symptoms enables earlier recognition and intervention. However, these signs can also indicate other mental health conditions, substance use, or normal developmental changes, making professional evaluation essential for accurate assessment.
First Episode Psychosis: Recognizing the Crisis
First episode psychosis represents the initial occurrence of positive symptoms requiring immediate clinical attention. The average time between symptom onset and treatment initiation ranges from 1-2 years, contributing to poorer long-term outcomes. Recognizing crisis situations enables appropriate emergency intervention.
Timeline of symptom development typically progresses from subtle prodromal changes to more obvious positive symptoms over weeks to months. Family members often report gradual escalation in concerning behaviors, followed by acute changes that prompt emergency intervention. Understanding this progression helps families seek help before crisis situations develop.
Emergency intervention indicators include expressing thoughts of self-harm or harm to others, complete inability to care for basic needs, severe agitation or unpredictable behavior, or complete loss of contact with reality. These situations require immediate emergency mental health evaluation, often through hospital emergency departments or mobile crisis teams.
Approaching someone experiencing symptoms requires patience, compassion, and safety awareness. Avoid arguing with delusions or hallucinations, instead acknowledging the person’s distress without agreeing with the content. Provide reassurance about safety and support while encouraging professional evaluation. Communication strategies learned through resources like resilience-building approaches can prove invaluable during these challenging conversations.
Early intervention programs specifically designed for first episode psychosis demonstrate remarkable effectiveness, with participants showing 50% better functional outcomes compared to traditional treatment approaches. These programs typically include rapid access to psychiatric care, family education and support, individual therapy, and assistance maintaining education or employment goals.
What Causes Schizophrenia?
Understanding schizophrenia’s causes helps reduce self-blame, family guilt, and public stigma while informing prevention and treatment strategies. Current research reveals complex interactions between genetic vulnerability, environmental factors, and neurodevelopmental processes rather than single causative factors.
Genetic Factors and Family History
Genetic research consistently demonstrates strong hereditary components in schizophrenia development, with heritability estimates reaching approximately 80%. This means genetic factors account for roughly 80% of schizophrenia risk, making it one of the most heritable mental health conditions. However, genetics alone do not determine destiny—environmental factors significantly influence whether genetic vulnerability develops into illness.
Heritability rates and family risk patterns reveal clear genetic influences. Children with one parent diagnosed with schizophrenia have approximately 10% risk of developing the condition, compared to 1% in the general population. When both parents are affected, risk increases to 40%. Siblings of people with schizophrenia face 8-10% risk, while identical twins show 40-50% concordance rates.
These statistics demonstrate that genetic factors create vulnerability rather than certainty. The majority of people with family history never develop schizophrenia, while some people with no known family history do develop the condition. This pattern suggests complex genetic mechanisms involving multiple genes rather than single gene inheritance.
Current genetic research identifies over 100 genetic variants associated with schizophrenia risk, each contributing small individual effects. Many of these variants also associate with other psychiatric conditions, explaining the frequent co-occurrence of mental health conditions within families. Genetic factors influence brain development, neurotransmitter systems, and immune function—all relevant to schizophrenia development.
Genetic testing limitations mean that current technology cannot predict individual schizophrenia risk accurately. Unlike single-gene disorders, schizophrenia involves complex interactions between multiple genetic variants and environmental factors. Genetic counseling can help families understand inheritance patterns and risk factors without providing definitive predictions about individual outcomes.
Environmental Triggers and Risk Factors
Environmental factors interact with genetic vulnerability to influence schizophrenia development. Understanding these factors helps identify prevention opportunities and explains why some genetically vulnerable individuals never develop symptoms while others do.
Prenatal infections and complications during pregnancy increase schizophrenia risk in offspring. Maternal influenza, toxoplasmosis, or other infections during critical brain development periods may trigger immune responses affecting fetal brain development. Birth complications involving oxygen deprivation also associate with increased risk, though the vast majority of people experiencing these complications never develop schizophrenia.
Childhood trauma and stress significantly increase risk for developing psychotic symptoms later in life. Physical abuse, sexual abuse, emotional neglect, or witnessing violence during childhood create lasting changes in stress response systems and brain development. However, trauma alone does not cause schizophrenia—it requires interaction with genetic vulnerability and other risk factors.
Substance use, particularly cannabis during adolescence, represents one of the most modifiable risk factors. Regular cannabis use before age 18 increases schizophrenia risk 2-3 times, with highest-potency products (high THC content) showing strongest associations. The developing adolescent brain appears particularly vulnerable to cannabis effects on dopamine systems and brain maturation processes.
Urban birth and migration stress demonstrate environmental influences on schizophrenia development. People born in urban areas show 2-3 times higher schizophrenia rates compared to rural areas. Immigration, particularly during childhood, also increases risk—possibly related to social stress, discrimination, or cultural adaptation challenges rather than geographic factors alone.
The Neurobiology Behind Schizophrenia
Modern neuroscience reveals schizophrenia as a neurodevelopmental condition involving multiple brain systems rather than single brain abnormalities. Understanding these neurobiological factors helps explain symptom patterns and guides treatment development.
The dopamine hypothesis evolution originally suggested that schizophrenia resulted from excessive dopamine activity. Current understanding recognizes more complex dopamine dysfunction involving hyperactivity in some brain regions (contributing to positive symptoms) and hypoactivity in others (contributing to negative and cognitive symptoms). This revised hypothesis explains why traditional antipsychotic medications effectively treat positive symptoms but show limited effects on negative and cognitive symptoms.
Brain structure differences identified through neuroimaging include enlarged ventricles (fluid-filled spaces), reduced gray matter in frontal and temporal regions, and altered connectivity between brain areas. These changes often appear before symptom onset and progress during illness course, supporting neurodevelopmental theories of schizophrenia causation.
Neurodevelopmental perspective proposes that schizophrenia results from disrupted brain development during prenatal and early postnatal periods, with symptoms emerging when affected brain circuits mature during adolescence and early adulthood. This theory explains the typical onset timing and suggests that early intervention during critical developmental periods might prevent or modify illness progression.
| Risk Factor | Relative Risk Increase | Modifiable? |
|---|---|---|
| Identical twin with schizophrenia | 40-50% lifetime risk | No |
| Both parents affected | 40% lifetime risk | No |
| Prenatal infection exposure | 2-3x baseline risk | Partially (vaccination, prenatal care) |
| Cannabis use during adolescence | 2-3x baseline risk | Yes (prevention, education) |
| Childhood trauma exposure | 2-3x baseline risk | Preventable (child protection, support) |
| Urban birth environment | 2-3x baseline risk | No (but urban stressors may be modifiable) |
This risk factor understanding emphasizes prevention opportunities through trauma prevention, substance abuse education, prenatal care improvement, and early intervention for people showing prodromal symptoms. While genetic factors cannot be changed, environmental modifications can significantly reduce overall risk.
Modern Treatment Approaches in 2025
Treatment for schizophrenia has undergone revolutionary changes in recent years, with 2024-2025 marking particularly significant advances in both pharmacological and psychosocial interventions. Modern approaches emphasize recovery, functioning, and quality of life rather than merely symptom control.
Breakthrough Medications and New Hope
The approval of KarXT (Cobenfy) by the FDA in September 2024 represents the first fundamentally new mechanism for treating schizophrenia in over three decades. Unlike traditional antipsychotics that primarily target dopamine systems, Cobenfy works through muscarinic and cholinergic pathways, offering hope for people who haven’t responded to conventional treatments.
Traditional antipsychotic medications fall into two categories: first-generation (typical) and second-generation (atypical) antipsychotics. First-generation medications like haloperidol and chlorpromazine effectively reduce positive symptoms but often cause significant side effects including movement disorders, sedation, and cognitive blunting. Second-generation medications like risperidone, olanzapine, and aripiprazole generally cause fewer movement-related side effects but may contribute to metabolic problems including weight gain and diabetes risk.
Cobenfy’s revolutionary approach targets muscarinic M1 and M4 receptors in the brain, providing a completely different therapeutic mechanism. Clinical trials demonstrate effectiveness for both positive and negative symptoms with a side effect profile distinct from traditional antipsychotics. Early reports suggest reduced risk of movement disorders, weight gain, and sedation—common limiting factors with existing medications.
Personalized medication approaches increasingly guide treatment selection based on individual factors including genetic testing, symptom patterns, side effect sensitivity, and previous treatment responses. Pharmacogenetic testing can identify people likely to experience specific side effects or require adjusted dosing based on genetic variations in drug metabolism.
Managing side effects remains crucial for treatment adherence and quality of life. Common approaches include switching medications when side effects prove intolerable, adding medications to counteract specific side effects, adjusting doses to minimize problems while maintaining effectiveness, and implementing lifestyle modifications to reduce side effect impact. Modern treatment emphasizes collaborative decision-making between individuals and their healthcare providers to optimize benefit-risk ratios.
Long-acting injectable formulations provide options for people who struggle with daily medication adherence, offering steady medication levels and reduced relapse risk. These formulations require injections every 2-4 weeks rather than daily pills, which can significantly improve treatment consistency.
Psychosocial Interventions That Work
While medications address neurobiological aspects of schizophrenia, psychosocial interventions target functional recovery, coping skills, and quality of life improvements. Research consistently demonstrates that combined medication and psychosocial treatment produces better outcomes than either approach alone.
Cognitive Behavioral Therapy for Psychosis (CBTp) represents the most extensively researched psychological intervention for schizophrenia. CBTp helps people develop coping strategies for persistent symptoms, challenge distressing beliefs, and improve problem-solving skills. Rather than eliminating hallucinations or delusions, CBTp often reduces their emotional impact and behavioral influence.
CBTp techniques include reality testing (examining evidence for beliefs), developing alternative explanations for experiences, coping strategy enhancement for managing distressing symptoms, and relapse prevention planning. Research shows 20-25% symptom reduction and improved functioning with 16-24 CBTp sessions.
Family therapy and education recognize that family support significantly impacts recovery outcomes. Family interventions reduce criticism and emotional over-involvement while increasing understanding, communication skills, and practical support. Studies demonstrate that family therapy reduces relapse rates by approximately 50% compared to medication alone.
Effective family programs include education about schizophrenia and treatment, communication skills training for managing difficult conversations, problem-solving techniques for addressing daily challenges, and stress management for family members’ wellbeing. Understanding the impact on family mental health, similar to approaches used in supporting children’s social, emotional and mental health needs, helps create supportive environments that benefit everyone involved.
Social skills training addresses interpersonal difficulties common in schizophrenia through structured learning approaches. Programs typically cover conversation skills, assertiveness training, conflict resolution, and workplace social interactions. Role-playing, video feedback, and homework assignments help people practice skills in real-world settings.
Vocational rehabilitation supports employment goals through specialized approaches addressing cognitive difficulties, symptom management, and workplace accommodations. Supported employment programs provide job coaches, employer education, and ongoing support to help people maintain competitive employment. Research shows 60-70% employment success rates with intensive vocational support.
Coordinated Specialty Care: The Gold Standard
Coordinated Specialty Care (CSC) represents an evidence-based approach specifically designed for people experiencing first episode psychosis. CSC programs demonstrate remarkable effectiveness, with participants showing 50% better functioning outcomes compared to traditional treatment approaches.
Early intervention program components integrate multiple services within coordinated teams including rapid access to psychiatric care (typically within 1-2 weeks), individual therapy focused on recovery goals, family education and support groups, case management assistance with practical needs, and peer support from people with lived experience.
Team-based approach ensures comprehensive care coordination through psychiatrists providing medication management, therapists delivering individual and group interventions, case managers assisting with housing, benefits, and daily living needs, vocational specialists supporting education and employment goals, and family therapists providing education and support.
Demonstrated outcomes from CSC programs include 50% better global functioning scores, reduced hospitalization rates and duration, higher rates of education and employment engagement, improved quality of life measures, and reduced family burden and distress. These programs typically serve people for 2-3 years during the critical early illness period.
CSC availability varies significantly by geographic location, with urban areas generally offering more program options than rural communities. The SAMHSA Early Serious Mental Illness Treatment Locator helps families identify local CSC programs and related resources.
Research consistently demonstrates that early intervention during the first few years after psychosis onset provides the greatest opportunity for recovery and prevents the functional decline traditionally associated with schizophrenia. This “critical period” approach emphasizes hope, recovery, and maintaining life goals rather than managing chronic disability.
Living Well with Schizophrenia: Recovery Stories
Recovery from schizophrenia encompasses much more than symptom reduction—it involves rebuilding meaningful life, pursuing personal goals, and contributing to communities. Modern understanding emphasizes that recovery represents an ongoing process rather than a fixed endpoint, with many people achieving fulfilling lives despite ongoing symptoms.
What Recovery Really Looks Like
Functional recovery versus clinical recovery represent two distinct but related concepts in schizophrenia treatment. Clinical recovery focuses on symptom reduction and medical stabilization, while functional recovery emphasizes returning to valued activities, relationships, and roles. Many people achieve functional recovery while experiencing some ongoing symptoms, challenging traditional assumptions about what “getting better” means.
Functional recovery might include returning to work or school, maintaining independent housing, developing meaningful relationships, pursuing hobbies and interests, contributing to family and community, and achieving personal goals. These accomplishments often prove more meaningful to individuals than complete symptom elimination.
Employment and education achievements demonstrate the potential for people with schizophrenia to pursue career and academic goals. With appropriate support, 60-70% of people can achieve competitive employment, while many others succeed in supported employment arrangements. Educational pursuits, including completing high school, attending college, or pursuing vocational training, remain achievable goals with proper accommodations and support.
Success stories include people becoming teachers, healthcare workers, business owners, artists, and community leaders. Many emphasize that work provides structure, purpose, social connection, and financial independence—all crucial for overall recovery and self-esteem.
Quality of life improvements encompass multiple domains including physical health, psychological wellbeing, social relationships, and environmental satisfaction. People in recovery often report increased life satisfaction, improved self-esteem, stronger relationships, better physical health, and greater optimism about the future.
Personal relationship success challenges stereotypes about people with schizophrenia being unable to maintain friendships, romantic partnerships, or family relationships. While relationships may require additional communication and understanding, many people develop strong, lasting connections. Some choose to disclose their diagnosis to trusted friends and partners, while others maintain privacy about their mental health status.
Daily Management Strategies
Successful daily management involves developing personalized strategies that account for individual symptoms, triggers, and life circumstances. Effective approaches typically combine medical treatment with practical coping skills and environmental modifications.
Medication adherence techniques address the reality that many people struggle with consistent medication use due to side effects, cognitive symptoms, or ambivalence about treatment. Successful strategies include using pill organizers or smartphone apps for reminders, connecting medication times to daily routines like meals, involving family members or friends in supportive accountability, addressing specific side effect concerns with healthcare providers, and understanding the connection between medication consistency and symptom stability.
Some people benefit from long-acting injectable medications that eliminate daily pill requirements, while others prefer splitting doses to minimize side effects or timing medications to reduce daytime sedation.
Stress management and coping skills prove essential for maintaining stability and preventing relapse. Effective stress management includes identifying personal stress triggers and early warning signs, developing relaxation techniques like deep breathing or progressive muscle relaxation, maintaining regular sleep schedules and healthy sleep hygiene, engaging in regular physical activity appropriate to individual fitness levels, and limiting alcohol and drug use that can worsen symptoms.
Many people develop personalized “wellness toolkits” including specific activities, people, or environments that promote stability and comfort during difficult periods.
Building support networks involves cultivating relationships that provide understanding, encouragement, and practical assistance. Support networks might include family members who understand the condition, friends who provide social connection and enjoyment, healthcare providers offering professional guidance, peer support groups with others who share similar experiences, and community members through work, volunteering, or hobbies.
Developing emotional intelligence skills, as explored in children’s emotional development resources, can enhance relationship-building and communication effectiveness for people managing mental health conditions.
Maintaining routine and structure helps manage cognitive symptoms and provides predictability that many people find comforting. Helpful routines include consistent wake and sleep times, regular meal schedules, scheduled medication times, planned daily activities or goals, and weekly structure for work, therapy, or social activities.
Flexibility within structure allows for adaptation during symptom fluctuations while maintaining helpful consistency.
Success Stories: Real People, Real Recovery
Recovery stories provide hope and practical insights while demonstrating the diversity of paths toward wellbeing. These examples represent composite stories based on common recovery experiences while protecting individual privacy.
Career achievements despite diagnosis illustrate the potential for professional success. Sarah, diagnosed at age 22 during her final year of college, initially dropped out due to hospitalizations and medication adjustments. With support from disability services, she completed her degree two years later and became a high school teacher. She now advocates for mental health awareness in educational settings while successfully managing her symptoms through medication, therapy, and workplace accommodations.
Michael experienced first episode psychosis at age 19 while working in construction. After stabilization and CSC program participation, he pursued computer programming training and now works as a software developer. He credits structured work environment, understanding supervisors, and consistent treatment for his success.
Family and relationship successes demonstrate that meaningful connections remain possible. Jennifer met her husband three years after her diagnosis. They married five years later and have two children. She emphasizes honest communication, family therapy, and mutual support as keys to their relationship success. Her husband became educated about schizophrenia and actively supports her treatment adherence and stress management.
David maintained close relationships with his siblings throughout his illness, though some friendships ended due to stigma and misunderstanding. He found new friendships through support groups and volunteer activities, building connections with people who appreciate his contributions rather than focusing on his diagnosis.
Community contributions highlight how people with schizophrenia enrich their communities through various roles. Maria became a peer support specialist, using her lived experience to help others navigate early recovery. Tom volunteers at a local animal shelter, finding that caring for animals provides purpose and routine while contributing to community welfare.
These stories emphasize that recovery looks different for each person but often includes meaningful activities, supportive relationships, and hope for the future.
| Timeline | Typical Recovery Milestones | Support Needed |
|---|---|---|
| 0-6 months | Symptom stabilization, safety, basic self-care | Intensive clinical support, family involvement, crisis planning |
| 6-18 months | Medication optimization, daily routine, social re-engagement | Continued therapy, skills training, family education |
| 1-3 years | Work/school re-entry, relationship building, independence skills | Vocational support, ongoing treatment, peer connections |
| 3+ years | Long-term goals, community involvement, advocacy | Maintenance treatment, continued growth, giving back |
This timeline represents typical patterns while acknowledging that recovery is highly individual. Some people achieve milestones more quickly, while others require additional time or follow different paths toward their goals.
Supporting a Loved One with Schizophrenia
Family members and friends play crucial roles in recovery outcomes, yet they often receive limited guidance about how to provide effective support while maintaining their own wellbeing. Understanding how to help while avoiding common pitfalls requires education, patience, and sometimes professional guidance.
Family Coping Strategies
Supporting someone with schizophrenia affects the entire family system, requiring adjustments in communication, expectations, and daily routines. Effective family coping strategies balance support with healthy boundaries while promoting everyone’s wellbeing.
Communication techniques for difficult conversations help families navigate challenging topics including medication adherence, symptom recognition, and future planning. Effective approaches include using “I” statements to express concerns without blame (“I feel worried when you don’t sleep” rather than “You’re not taking care of yourself”), validating emotions while addressing problematic behaviors (“I understand you’re frustrated, and we need to find a solution”), avoiding arguing with delusions or hallucinations while acknowledging distress, and choosing appropriate timing for important discussions when the person feels calm and receptive.
Learning to distinguish between symptom-related behaviors and personal choices helps families respond appropriately without enabling or creating unnecessary conflict. Professional family therapy can provide guided practice with these communication skills in a supportive environment.
Setting healthy boundaries protects family wellbeing while maintaining supportive relationships. Healthy boundaries might include requiring treatment engagement for continued financial support, establishing house rules about medication compliance and substance use, maintaining personal activities and relationships outside the caregiving role, and seeking professional help for safety concerns rather than managing crises alone.
Boundaries differ from ultimatums—they represent consistent expectations with natural consequences rather than punitive threats.
Self-care for caregivers acknowledges that family members need support and respite to provide sustainable help. Caregiver self-care includes maintaining personal health through regular medical care, exercise, and nutrition, preserving relationships and activities that provide enjoyment and stress relief, seeking education about schizophrenia and treatment options, joining family support groups for emotional support and practical advice, and considering individual therapy for processing emotions and developing coping strategies.
Research shows that caregiver burnout contributes to family breakdown and poorer outcomes for people with schizophrenia, making family self-care an essential component of comprehensive treatment.
Managing crisis situations requires advance planning and clear protocols for handling emergencies. Crisis planning includes identifying early warning signs of symptom escalation, developing action plans for different levels of concern, maintaining emergency contact information for healthcare providers and crisis services, understanding when to seek emergency intervention versus outpatient care, and involving the person with schizophrenia in crisis planning when they’re stable.
Many families benefit from creating written crisis plans that outline specific steps, contact information, and decision-making criteria for various situations.
Practical Support and Resources
Navigating the complex systems involved in mental healthcare, disability benefits, and community resources often overwhelms families. Understanding available resources and how to access them provides crucial practical support.
Navigating healthcare systems involves understanding insurance coverage, finding qualified providers, and advocating for appropriate care. Practical steps include verifying mental health coverage including inpatient, outpatient, and prescription benefits, researching providers who specialize in schizophrenia treatment and accept the person’s insurance, understanding how to access crisis services and emergency care, and learning about patient rights and how to file grievances when necessary.
Many insurance plans require prior authorization for certain medications or treatments, making it important to understand these processes and plan accordingly.
Financial planning and benefits help families address the economic impact of schizophrenia including treatment costs and potential work limitations. Relevant resources include Social Security Disability Insurance (SSDI) for people with work histories, Supplemental Security Income (SSI) for people with limited work histories, Medicaid for healthcare coverage, housing assistance programs, and vocational rehabilitation services.
Applying for benefits often requires extensive documentation and can take months or years, making early application important even if the person initially hopes to return to work quickly.
Legal considerations and guardianship become relevant when people cannot make safe decisions about their care. Legal options include power of attorney arrangements made when the person has decision-making capacity, guardianship proceedings for people who lack capacity to make important decisions, advance psychiatric directives that specify treatment preferences, and understanding involuntary commitment laws and procedures.
These legal tools should be used thoughtfully and preferably with the person’s input when possible, as they significantly impact autonomy and self-determination.
Finding local support groups provides emotional support and practical advice from other families facing similar challenges. Support groups offer education about schizophrenia and treatment, emotional support from people who understand the experience, practical advice about navigating systems and resources, and advocacy opportunities for improved services and reduced stigma.
The National Alliance on Mental Illness (NAMI) provides family support groups, educational programs, and advocacy opportunities in most communities. Online support groups offer additional options for families in areas with limited local resources.
Understanding family mental health needs through resources that address emotional intelligence and family communication can strengthen family resilience and improve overall outcomes for everyone involved.
Looking Forward: Hope and Research
The future of schizophrenia treatment holds unprecedented promise, with multiple breakthrough developments in research, treatment, and social understanding converging to improve outcomes for millions of people worldwide. Current research directions suggest that the next decade will bring transformative changes in how we prevent, treat, and understand this complex condition.
Emerging treatments on the horizon include several revolutionary approaches currently in clinical trials. Glutamate-targeting medications represent a promising new class of treatments that address different brain systems than traditional dopamine-focused medications. These treatments may prove particularly effective for cognitive and negative symptoms that respond poorly to current medications.
Neuroplasticity-based interventions use targeted brain training and stimulation techniques to strengthen neural connections affected by schizophrenia. Transcranial magnetic stimulation (TMS) and cognitive enhancement therapy show promise for improving cognitive functioning and reducing negative symptoms through brain training approaches.
Research into prevention focuses on identifying and intervening with people during prodromal phases before full psychosis develops. Early intervention programs now include specialized services for people showing early warning signs, with some studies suggesting that intensive support during this period can delay or prevent psychosis onset in vulnerable individuals.
Environmental prevention strategies target modifiable risk factors including reducing childhood trauma through improved child protection and family support, substance abuse prevention programs tailored for adolescents at higher genetic risk, prenatal care improvements to reduce infection and birth complication risks, and urban planning approaches that reduce environmental stressors associated with increased psychosis risk.
Reducing stigma and improving outcomes requires continued public education, policy changes, and cultural shifts in how society understands and responds to mental health conditions. Anti-stigma campaigns increasingly feature people with lived experience sharing their recovery stories, challenging stereotypes and demonstrating the potential for meaningful, productive lives.
Employment and housing discrimination protections continue expanding, while educational initiatives in schools, workplaces, and healthcare settings promote understanding and inclusion. Media representation of mental health conditions gradually improves, moving away from sensationalized portrayals toward more accurate, hope-focused narratives.
The importance of early intervention cannot be overstated in shaping future outcomes. Research consistently demonstrates that people receiving appropriate treatment within the first two years of symptom onset achieve dramatically better long-term functioning, reduced hospitalization needs, and maintained education and employment engagement.
Investment in early intervention programs, public education about warning signs, and reduced barriers to mental healthcare access represent crucial steps toward improving outcomes for future generations. Understanding that recovery is not only possible but probable with appropriate support helps families and individuals maintain hope during challenging periods.
The convergence of medical advances, psychosocial innovations, and changing social attitudes creates an environment of unprecedented opportunity for people affected by schizophrenia. While challenges remain, the trajectory clearly points toward improved treatments, reduced stigma, and greater recognition of the potential for recovery and meaningful life engagement.
Conclusion
Schizophrenia represents a complex but treatable neurobiological condition affecting millions worldwide. While the journey involves challenges, modern understanding emphasizes recovery, hope, and the potential for meaningful life engagement. Breakthrough treatments like Cobenfy, coordinated specialty care programs, and comprehensive psychosocial interventions offer unprecedented opportunities for positive outcomes.
Recovery statistics tell a powerful story: 25% of people achieve complete recovery, while 50% experience significant improvement. Early intervention proves crucial, with people receiving treatment within two years of symptom onset showing dramatically better long-term functioning.
The path forward requires continued investment in research, early intervention programs, family support, and stigma reduction. Understanding schizophrenia as a medical condition rather than a character flaw empowers individuals, families, and communities to provide appropriate support while maintaining hope for the future.
For anyone affected by schizophrenia—whether personally or through a loved one—remember that recovery is not only possible but probable with appropriate treatment and support. The convergence of medical advances, social understanding, and recovery-focused approaches creates an environment of unprecedented opportunity.
Frequently Asked Questions
What is it like having schizophrenia?
Living with schizophrenia varies greatly between individuals, but many describe it as experiencing altered perceptions of reality through hallucinations or delusions. Daily life often involves managing symptoms through medication and therapy while working toward personal goals. With proper treatment, many people maintain relationships, employment, and independence. The experience improves significantly with early intervention and comprehensive support systems.
What are 5 symptoms of schizophrenia?
The five main symptoms include hallucinations (typically hearing voices), delusions (false beliefs), disorganized thinking and speech, reduced emotional expression, and cognitive difficulties like memory problems. Positive symptoms add experiences not normally present, while negative symptoms reduce normal functioning. Cognitive symptoms affect concentration and decision-making. These symptoms vary in intensity and respond differently to treatment approaches.
How do you talk to someone with schizophrenia?
Communicate with patience, respect, and empathy. Avoid arguing with delusions or hallucinations—instead acknowledge their distress without agreeing with the content. Use clear, simple language and maintain a calm tone. Listen actively and validate their feelings while encouraging treatment adherence. Avoid making sudden movements or raising your voice. Focus on their strengths and recovery goals rather than dwelling on symptoms.
What triggers schizophrenia?
Schizophrenia develops through complex interactions between genetic vulnerability and environmental factors. Common triggers include high stress levels, substance use (particularly cannabis during adolescence), social isolation, major life changes, and lack of sleep. Prenatal factors like maternal infections and birth complications also increase risk. However, triggers vary individually—what affects one person may not impact another with different genetic predispositions.
Can schizophrenia be cured?
While there’s no cure for schizophrenia, it’s highly treatable with significant recovery potential. Twenty-five percent achieve complete recovery, and 75% show substantial improvement with proper treatment. Modern approaches focus on symptom management, functional recovery, and quality of life rather than cure. Breakthrough medications like Cobenfy and coordinated specialty care programs demonstrate unprecedented effectiveness for helping people achieve their life goals.
Is schizophrenia hereditary?
Schizophrenia has strong genetic components with 80% heritability, but genetics alone don’t determine outcomes. Children with one affected parent have 10% risk versus 1% general population risk. Identical twins show 40-50% concordance, meaning genetics create vulnerability rather than certainty. Environmental factors significantly influence whether genetic predisposition develops into illness. Most people with family history never develop schizophrenia.
How is schizophrenia diagnosed?
Diagnosis requires comprehensive psychiatric evaluation by qualified mental health professionals. No single test exists—doctors assess symptom patterns, duration, and functional impact. Symptoms must persist for at least six months and significantly impair functioning. The process includes medical examination to rule out other conditions, psychological assessment, and sometimes brain imaging. Early intervention programs can provide support even before full diagnosis criteria are met.
What should you not say to someone with schizophrenia?
Avoid dismissive phrases like “just ignore the voices” or “it’s all in your head.” Don’t argue with their reality or demand they admit delusions are false. Avoid stigmatizing language or treating them differently because of their diagnosis. Don’t blame them for their condition or suggest they could “get better if they tried harder.” Instead, offer support, encourage treatment, and focus on their strengths and recovery progress.
References
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.).
Barch, D. M., & Ceaser, A. (2012). Cognition in schizophrenia: Core psychological and neural mechanisms. Trends in Cognitive Sciences, 16(1), 27-34.
Dixon, L. B., Dickerson, F., Bellack, A. S., Bennett, M., Dickinson, D., Goldberg, R. W., … & Kreyenbuhl, J. (2010). The 2009 PORT psychosocial treatment recommendations and summary statements. Schizophrenia Bulletin, 36(1), 48-70.
Goleman, D. (1995). Emotional intelligence: Why it matters more than IQ. Bantam Books.
Hull, L., Petrides, K. V., Allison, C., Smith, P., Baron-Cohen, S., Lai, M. C., & Mandy, W. (2017). “Putting on my best normal”: Social camouflaging in adults with autism spectrum conditions. Journal of Autism and Developmental Disorders, 47(8), 2519-2534.
Kane, J. M., Schooler, N. R., Marcy, P., Correll, C. U., Brunette, M. F., Mueser, K. T., … & Robinson, D. G. (2020). The RAISE early treatment program for first-episode psychosis: Background, rationale, and study design. Journal of Clinical Psychiatry, 81(6), 19r13120.
Leucht, S., Cipriani, A., Spineli, L., Mavridis, D., Örey, D., Richter, F., … & Davis, J. M. (2013). Comparative efficacy and tolerability of 15 antipsychotic drugs in schizophrenia: A multiple-treatments meta-analysis. The Lancet, 382(9896), 951-962.
Lieberman, J. A., Stroup, T. S., McEvoy, J. P., Swartz, M. S., Rosenheck, R. A., Perkins, D. O., … & Hsiao, J. K. (2005). Effectiveness of antipsychotic drugs in patients with chronic schizophrenia. New England Journal of Medicine, 353(12), 1209-1223.
McGrath, J., Saha, S., Chant, D., & Welham, J. (2008). Schizophrenia: A concise overview of incidence, prevalence, and mortality. Epidemiologic Reviews, 30(1), 67-76.
Salovey, P., & Mayer, J. D. (1990). Emotional intelligence. Imagination, Cognition and Personality, 9(3), 185-211.
Schooler, N., Rabinowitz, J., Davidson, M., Emsley, R., Harvey, P. D., Kopala, L., … & Strom, B. L. (2005). Risperidone and haloperidol in first-episode psychosis: A long-term randomized trial. American Journal of Psychiatry, 162(5), 947-953.
van Os, J., & Kapur, S. (2009). Schizophrenia. The Lancet, 374(9690), 635-645.
Wykes, T., Huddy, V., Cellard, C., McGurk, S. R., & Czobor, P. (2011). A meta-analysis of cognitive remediation for schizophrenia: Methodology and effect sizes. American Journal of Psychiatry, 168(5), 472-485.
Further Reading and Research
Recommended Articles
- Barch, D. M., & Sheffield, J. M. (2014). Cognitive impairments in psychotic disorders: Common mechanisms and measurement. World Psychiatry, 13(3), 224-232.
- Correll, C. U., Rubio, J. M., Inczedy-Farkas, G., Birnbaum, M. L., Kane, J. M., & Leucht, S. (2017). Efficacy of 42 pharmacologic cotreatment strategies added to antipsychotic monotherapy in schizophrenia: Systematic overview and quality appraisal of the meta-analytic evidence. JAMA Psychiatry, 74(7), 675-684.
- Harvey, P. D., & Bowie, C. R. (2013). Cognitive enhancement in schizophrenia: Pharmacological and cognitive remediation approaches. Psychiatric Clinics of North America, 36(3), 377-390.
Suggested Books
- Amador, X. (2012). I Am Not Sick, I Don’t Need Help! How to Help Someone with Mental Illness Accept Treatment.
- Practical guide for families learning to communicate with loved ones who lack insight into their mental illness, providing specific techniques for building therapeutic relationships.
- Torrey, E. F. (2019). Surviving Schizophrenia: A Family Manual (7th ed.).
- Comprehensive resource covering symptoms, treatment options, and practical advice for families, updated with latest research and treatment approaches.
- Keefe, R. S., & Harvey, P. D. (2012). Cognitive Impairment in Schizophrenia: Characteristics, Assessment and Treatment.
- Academic text exploring cognitive symptoms, assessment methods, and evidence-based interventions for cognitive enhancement in schizophrenia treatment.
Recommended Websites
- National Alliance on Mental Illness (NAMI)
- Comprehensive mental health resources including support groups, educational programs, advocacy opportunities, and crisis intervention information for individuals and families.
- Substance Abuse and Mental Health Services Administration (SAMHSA)
- Federal agency providing treatment locators, crisis resources, prevention programs, and evidence-based practice guidelines for mental health and substance abuse treatment.
- Schizophrenia and Related Disorders Alliance of America (SARDAA)
- Specialized organization offering support groups, educational materials, research updates, and advocacy specifically focused on schizophrenia and related psychotic disorders.
To cite this article please use:
Early Years TV Schizophrenia Complete Guide: Symptoms, Causes and Recovery. Available at: https://www.earlyyears.tv/schizophrenia-complete-guide-symptoms-causes-recovery/ (Accessed: 13 November 2025).


