The Endocrine System: Hormones and Behavior Connection
A single hormone surge can alter your decision-making within minutes, influence who you’re attracted to, determine how well you sleep tonight, and even affect whether you remember this information tomorrow—yet most people remain unaware of these powerful chemical messengers constantly shaping their daily experiences.
Key Takeaways:
- How do hormones affect behavior? Hormones create bidirectional relationships with behavior—they influence how you think and act, while your behaviors and experiences actively shape hormone production, creating dynamic feedback loops throughout your day.
Introduction
Every day, your body orchestrates an intricate symphony of chemical messengers that influence everything from your morning alertness to your evening wind-down routine. These chemical messengers—hormones—don’t just regulate basic body functions like hunger and sleep. They profoundly shape how you think, feel, and behave in ways you might never have imagined.
Behavioral endocrinology, the scientific study of hormone-behavior relationships, reveals that these chemical signals create a constant two-way conversation between your body and brain. Understanding neuroscience and early brain development helps us appreciate how hormones influence neural pathways from our earliest years, while recognizing the importance of self-regulation in the early years shows us how hormonal systems develop alongside our emotional control abilities.
This comprehensive guide examines how hormones influence behavior across the lifespan, from the stress response that helped our ancestors survive threats to the complex social bonds that define modern human relationships. Whether you’re a psychology student seeking to understand biological influences on behavior, a parent curious about your teenager’s mood swings, or simply someone interested in the fascinating connections between body and mind, you’ll discover how your hormonal system shapes every aspect of your daily experience.
Understanding Your Body’s Chemical Messengers
What Are Hormones and How Do They Work?
Hormones are specialized chemical messengers produced by your endocrine glands and released directly into your bloodstream. Unlike neurotransmitters that communicate across tiny synapses between nerve cells, hormones travel throughout your entire body, creating widespread effects that can last from minutes to hours or even influence you for years.
Think of hormones as your body’s internal postal service, delivering specific messages to particular destinations. Each hormone has a unique chemical structure that allows it to “unlock” specific receptor sites on target cells, much like a key fitting into a lock. When a hormone binds to its receptor, it triggers a cascade of cellular changes that ultimately influence your thoughts, emotions, and behaviors.
The key difference between hormones and neurotransmitters lies in their scope and duration. While neurotransmitters create rapid, localized effects lasting milliseconds, hormones produce slower, more sustained changes throughout your system. This explains why you might feel anxious for hours after a stressful event (due to circulating cortisol) even after the immediate threat has passed.
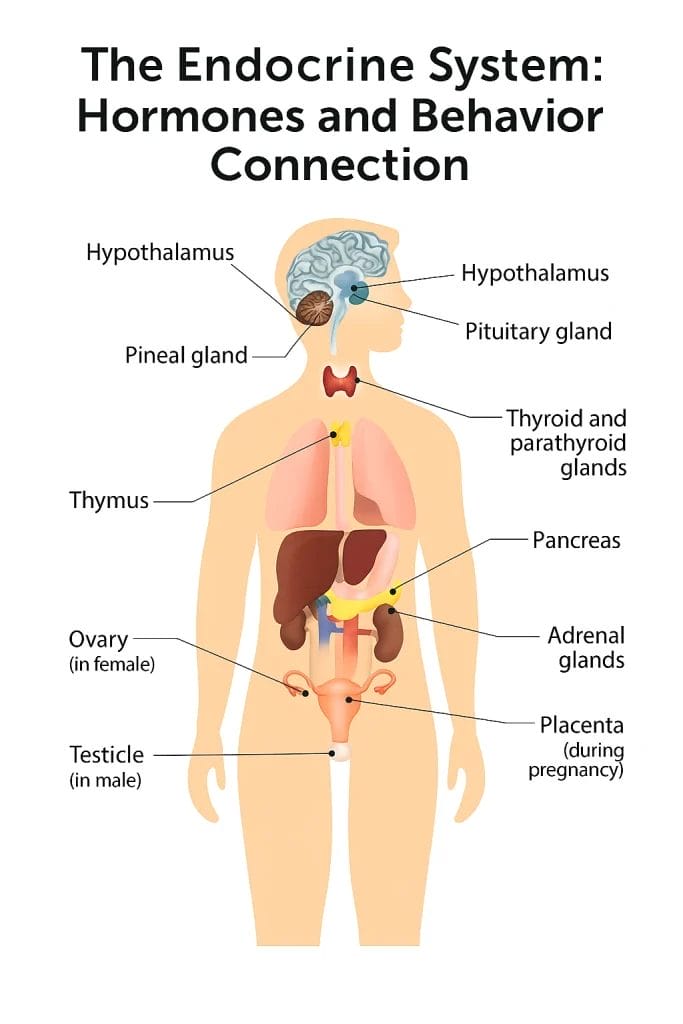
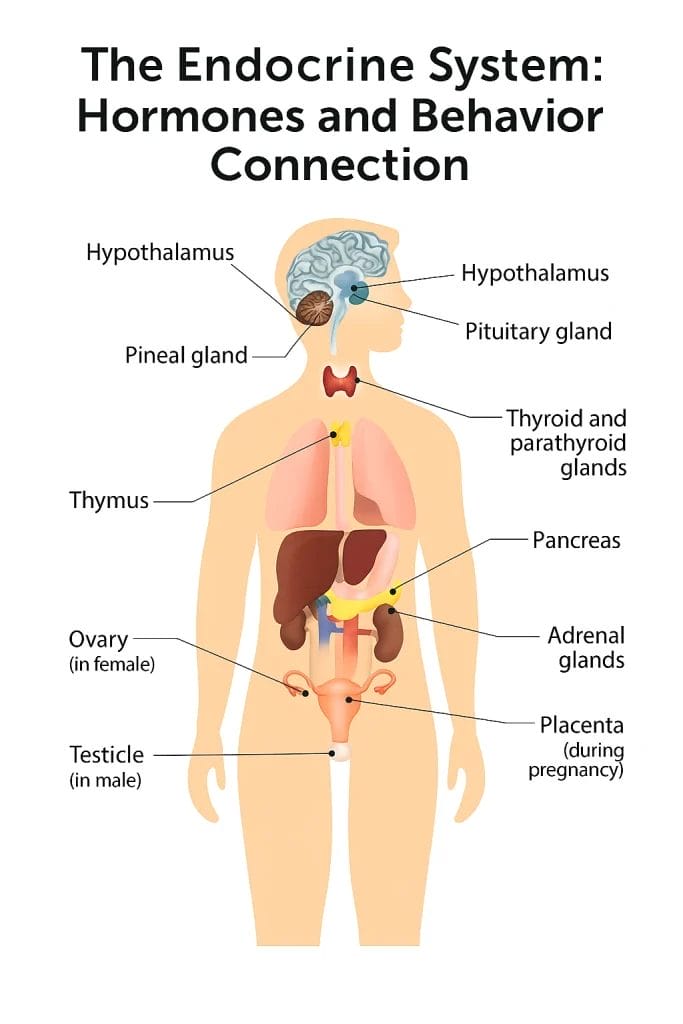
Image based on information from https://www.epa.gov/endocrine-disruption/overview-endocrine-system
The Endocrine System: Your Body’s Control Network
Your endocrine system consists of several specialized glands distributed throughout your body, each producing specific hormones with distinct behavioral effects. Understanding these major players helps explain the complex relationships between your physical state and psychological experience.
The hypothalamus serves as the master coordinator, connecting your nervous and endocrine systems. This small brain region monitors your internal state and external environment, triggering hormone release in response to everything from stress to social interactions. When you encounter a potential threat, your hypothalamus initiates the stress response cascade that affects your behavior within seconds.
Your pituitary gland, often called the “master gland,” receives signals from the hypothalamus and releases hormones that control other endocrine glands. This hierarchical system ensures coordinated responses throughout your body. The thyroid regulates your metabolic rate and energy levels, influencing how active and alert you feel. Your adrenal glands produce cortisol and adrenaline, the primary stress hormones that dramatically alter your behavior during challenging situations.
Table 1: Major Endocrine Glands and Their Primary Functions
| Gland | Primary Hormones | Key Behaviors Influenced |
|---|---|---|
| Hypothalamus | Releasing/inhibiting hormones | Sleep-wake cycles, appetite, social bonding |
| Pituitary | Growth hormone, oxytocin, vasopressin | Social behavior, trust, pair bonding |
| Thyroid | T3, T4 | Energy levels, mood, cognitive speed |
| Adrenals | Cortisol, adrenaline, aldosterone | Stress response, aggression, memory formation |
| Ovaries/Testes | Estrogen, progesterone, testosterone | Sexual behavior, aggression, social dominance |
| Pancreas | Insulin, glucagon | Hunger, mood stability, energy regulation |
Feedback mechanisms maintain hormonal balance through negative feedback loops, similar to a thermostat regulating temperature. When hormone levels reach their target range, the system reduces production. When levels drop too low, production increases. This self-regulating system normally keeps your hormones within healthy ranges, but stress, illness, or environmental factors can disrupt these delicate balances, leading to behavioral changes.
As neuroscience expert Debbie Garvey explains, understanding how hormones like cortisol and adrenaline affect the developing brain helps us appreciate why children sometimes struggle with emotional regulation and need adult support to manage their responses.
The Science Behind Hormone-Behavior Connections
Two-Way Streets: How Hormones and Behavior Influence Each Other
One of the most fascinating aspects of behavioral endocrinology is the bidirectional relationship between hormones and behavior. Not only do hormones influence how you act, but your behaviors and experiences actively shape your hormonal responses. This creates dynamic feedback loops that can either reinforce positive patterns or maintain problematic cycles.
Organizational effects occur during critical developmental periods when hormones permanently shape brain structure and function. During prenatal development, for example, testosterone exposure influences the formation of neural circuits related to spatial ability, aggression, and social behavior. These early hormonal influences create lasting differences in how individuals respond to similar situations throughout their lives.
Activational effects represent the immediate influence of circulating hormones on existing brain circuits. Unlike organizational effects, these changes are temporary and reversible. When your testosterone levels fluctuate throughout the day or across seasons, they temporarily activate or suppress certain behavioral tendencies without permanently altering brain structure.
Environmental factors continuously influence your hormonal production through complex interactions between your genes and experiences. Social situations, physical challenges, seasonal changes, and even the foods you eat can trigger hormonal responses that shape your behavior. This explains why the same person might respond very differently to similar situations depending on their current hormonal state and recent experiences.
Research in psychoneuroendocrinology—the study of interactions between psychological processes, the nervous system, and the endocrine system—reveals that chronic stress can reshape your brain’s response to future stressors. Prolonged elevation of cortisol actually changes the structure of brain regions involved in memory and emotional regulation, creating lasting impacts on behavior that persist long after the original stressful experience ends.
Measuring Hormones in Research
Understanding hormone-behavior relationships requires sophisticated measurement techniques that can capture the dynamic nature of hormonal systems. Modern research uses multiple approaches to assess hormonal influences on behavior, each with distinct advantages and limitations.
Saliva testing has revolutionized hormonal research by providing a non-invasive method for measuring “free” hormones—the biologically active portion not bound to proteins in your blood. Saliva samples can be collected repeatedly throughout the day, allowing researchers to track natural hormonal rhythms and responses to specific events. This technique has revealed how cortisol patterns change in response to social challenges, romantic relationships, and even competitive sports.
Blood sampling remains the gold standard for measuring total hormone concentrations, but it provides only a snapshot of hormone levels at a single moment. Since many hormones fluctuate rapidly throughout the day, single blood samples may miss important patterns or responses to environmental changes. Additionally, the stress of blood draws can itself alter hormone levels, potentially confounding research results.
Hair analysis offers a unique window into long-term hormonal exposure by capturing average hormone levels over the past 2-3 months. This approach is particularly valuable for studying chronic conditions or the cumulative effects of prolonged stress. However, hair analysis cannot reveal short-term fluctuations or rapid responses to specific events.
The complexity of hormonal systems creates significant challenges for researchers trying to establish causal relationships between hormones and behavior. Hormones rarely act in isolation—they interact with each other, with neurotransmitter systems, and with environmental factors in ways that can either amplify or dampen their effects. A behavior that appears to be caused by a single hormone might actually result from complex interactions between multiple hormonal systems.
Correlation versus causation represents perhaps the biggest challenge in hormonal research. While we might observe that people with higher testosterone levels show more aggressive behavior, this doesn’t necessarily mean testosterone causes aggression. The relationship could be reversed (aggressive behavior increases testosterone), or both could be influenced by a third factor such as social status or genetic variation.
Stress Hormones and Your Daily Behavior
The HPA Axis: Your Body’s Alarm System
The hypothalamic-pituitary-adrenal (HPA) axis represents your body’s primary stress response system, orchestrating behavioral changes that have helped humans survive threats for thousands of years. Understanding how this system works provides crucial insights into everything from workplace performance to relationships and mental health.
When your brain perceives a potential threat—whether physical danger, social rejection, or academic pressure—your hypothalamus releases corticotropin-releasing hormone (CRH) within seconds. This chemical signal travels to your pituitary gland, which responds by releasing adrenocorticotropic hormone (ACTH) into your bloodstream. ACTH then stimulates your adrenal glands to produce cortisol, the primary stress hormone that creates widespread behavioral changes.
This cascade typically takes 15-30 minutes to reach peak activation, which explains why you might continue feeling stressed long after the initial trigger has passed. The system evolved to maintain vigilance until threats completely disappeared—a useful adaptation when facing predators, but potentially problematic in modern environments where stressors are often psychological and persistent.
Acute stress responses prepare your body for immediate action through the release of adrenaline (epinephrine) and noradrenaline (norepinephrine). These hormones increase your heart rate, sharpen your focus, and redirect energy toward your muscles. Behaviorally, you become more alert, reactive, and ready for physical action. This “fight-or-flight” response can enhance performance during short-term challenges like presentations, athletic competitions, or emergency situations.
Chronic stress creates very different behavioral effects through prolonged cortisol elevation. While acute stress enhances certain cognitive abilities, chronic stress impairs memory formation, reduces cognitive flexibility, and increases emotional reactivity. People experiencing chronic stress often report difficulty concentrating, increased irritability, and problems with decision-making—all direct consequences of sustained hormonal activation.
The relationship between stress and early childhood anxiety demonstrates how these systems develop over time, with early experiences shaping long-term stress responsivity and emotional regulation abilities.
How Stress Hormones Change Your Actions
Cortisol influences behavior through direct effects on multiple brain regions involved in cognition, emotion, and social behavior. The hippocampus, crucial for memory formation, contains high concentrations of cortisol receptors. Moderate cortisol levels enhance memory consolidation, helping you remember important events more clearly. However, excessive cortisol impairs hippocampal function, leading to memory problems and difficulty learning new information.
The prefrontal cortex, responsible for executive functions like planning and impulse control, shows reduced activity during chronic stress. This explains why stressed individuals often struggle with decision-making, have trouble prioritizing tasks, and may act more impulsively than usual. The combination of impaired memory and reduced executive control creates a particularly challenging situation for students and professionals dealing with ongoing stress.
Cortisol also affects the amygdala, your brain’s “threat detection center,” making you more sensitive to potential dangers in your environment. This heightened vigilance can be useful in genuinely threatening situations, but it can also lead to overreactions to minor stressors. People with chronic stress often report feeling “on edge” or having difficulty relaxing, even in safe environments.
Social behavior changes significantly under stress hormonal influence. Cortisol can increase social anxiety and reduce empathy, making it harder to read others’ emotional states accurately. At the same time, stress can increase your need for social support, creating an internal conflict between wanting connection and feeling less capable of maintaining positive relationships.
Table 2: Cortisol Levels and Behavioral Effects
| Cortisol Level | Time Frame | Behavioral Effects | Adaptive Value |
|---|---|---|---|
| Baseline | Daily rhythm | Normal mood, good memory | Maintains basic functions |
| Moderately elevated | Acute stress (minutes to hours) | Enhanced alertness, improved memory consolidation | Helps handle challenges |
| Highly elevated | Severe acute stress | Fight-or-flight response, tunnel vision | Survival response |
| Chronically elevated | Weeks to months | Memory problems, reduced empathy, irritability | Maladaptive in modern contexts |
Individual differences in stress responsivity partially explain why people react so differently to similar challenges. Some individuals have naturally more sensitive HPA axes that respond strongly to minor stressors, while others remain relatively calm under significant pressure. These differences result from complex interactions between genetic factors, early life experiences, and ongoing environmental influences.
Sleep quality profoundly affects cortisol patterns and stress responsivity. Normal cortisol follows a daily rhythm, with levels highest in the morning to promote wakefulness and gradually declining throughout the day. Disrupted sleep can flatten this natural rhythm, leading to elevated evening cortisol that interferes with relaxation and sleep quality, creating a vicious cycle of stress and poor rest.
Sex Hormones and Social Behavior
Testosterone: Beyond Aggression Myths
Popular culture often portrays testosterone as the “aggression hormone,” but scientific research reveals a much more nuanced relationship between this hormone and social behavior. While testosterone does influence competitive and assertive behaviors, its effects are highly dependent on social context, individual personality, and cultural factors.
Testosterone levels fluctuate naturally throughout the day, across seasons, and in response to social situations. Men typically show peak testosterone in the morning with gradual decline throughout the day, while women experience more complex patterns related to their menstrual cycles. These fluctuations create corresponding changes in mood, confidence, and social behavior that many people recognize in themselves and others.
Competition increases testosterone in both men and women, but the magnitude and duration of these increases depend on the outcome and the individual’s investment in success. Winners of competitive interactions often show sustained testosterone elevation for hours or even days, while losers typically experience decreases. This “winner effect” can create positive feedback loops where success breeds confidence and further success, or negative cycles where failures reduce confidence and future performance.
The relationship between testosterone and aggression is more complex than many assume. Rather than causing indiscriminate aggression, testosterone appears to motivate behaviors aimed at maintaining or improving social status. In some contexts, this might involve physical aggression, but in most modern situations, it manifests as assertiveness, competitiveness, or leadership behavior. Successful business leaders and athletes often have relatively high testosterone levels, but they channel these impulses into socially acceptable forms of competition.
Testosterone influences cognitive abilities in subtle but measurable ways. Higher testosterone levels are associated with enhanced spatial abilities, faster processing of certain types of visual information, and increased confidence in decision-making. However, extremely high levels can impair cognitive flexibility and increase impulsive behavior. The optimal level appears to be moderate rather than maximal.
Estrogen and Progesterone: Mood and Social Connection
Estrogen and progesterone create complex behavioral effects that vary dramatically across the menstrual cycle, pregnancy, and menopause. These hormones don’t just influence reproductive behavior—they affect mood regulation, social bonding, cognitive performance, and stress responsivity in sophisticated ways that researchers are still discovering.
Estrogen enhances verbal abilities and social cognition, making it easier to read others’ emotions and communicate effectively. Women often report feeling more socially confident and articulate during the first half of their menstrual cycle when estrogen levels are rising. This hormone also improves certain types of memory, particularly verbal memory and the ability to remember emotional events.
The social bonding effects of estrogen appear to work through interactions with oxytocin and other social hormones. Higher estrogen levels increase sensitivity to oxytocin, enhancing feelings of trust and connection with others. This might explain why many women feel more sociable and emotionally open during certain phases of their cycle.
Progesterone, often called the “calming hormone,” has anxiety-reducing effects that become particularly noticeable during pregnancy when levels increase dramatically. However, progesterone can also cause drowsiness and reduce cognitive performance on some tasks. The rapid decline in progesterone after menstruation or childbirth can contribute to mood changes and increased stress sensitivity.
The interaction between estrogen and progesterone creates the characteristic emotional and behavioral changes that many women experience across their cycles. The premenstrual period, when both hormones decline rapidly, often involves increased stress sensitivity, emotional reactivity, and social withdrawal. Understanding these patterns can help women anticipate and manage cyclical changes in mood and behavior.
The Role of Environment and Society
Hormonal effects on behavior are significantly modified by cultural and environmental factors. The same hormone level might produce very different behaviors depending on social expectations, cultural norms, and individual learning experiences. This interaction between biology and environment helps explain why hormonal influences vary across different societies and historical periods.
Social context powerfully influences hormonal responses to competitive situations. Research shows that testosterone responses to competition are much stronger when the competition occurs in front of an audience or when the stakes are personally meaningful. This suggests that hormones amplify behaviorally relevant situations rather than creating uniform responses regardless of context.
Cultural definitions of appropriate behavior shape how hormonal influences are expressed. In cultures that encourage direct competition and individual achievement, testosterone might lead to more obvious competitive behaviors. In cultures emphasizing cooperation and group harmony, the same hormonal levels might manifest as leadership or protective behaviors rather than overt aggression.
Individual personality traits interact with hormones to determine behavioral outcomes. People high in trait aggression show stronger behavioral responses to testosterone changes, while those high in empathy might show enhanced prosocial behaviors during hormonal fluctuations. This helps explain why hormone levels alone cannot predict behavior—the interaction between hormones and personality creates unique patterns for each individual.
Environmental stressors can disrupt normal hormonal patterns and alter their behavioral effects. Chronic stress, poor nutrition, inadequate sleep, and exposure to endocrine-disrupting chemicals can all interfere with normal hormone production and signaling, potentially reducing the adaptive value of hormonal responses to social situations.
Development and Life Stages
Hormones Shape Us Before Birth
The hormonal environment during prenatal development creates lasting effects on brain structure and behavior that persist throughout life. Understanding these early influences helps explain individual differences in everything from spatial abilities to emotional regulation and social preferences.
Testosterone exposure in the womb significantly influences brain development, creating sex differences in neural structure that affect behavior from infancy onward. Higher prenatal testosterone exposure is associated with enhanced spatial abilities, increased preference for physical play, and greater interest in mechanical objects. These effects occur regardless of biological sex—girls exposed to higher testosterone levels in utero often show more “masculine” play preferences and cognitive patterns.
The timing of prenatal hormone exposure is crucial. Different brain regions develop at different times during pregnancy, creating critical periods when hormonal influences have maximum impact. Early exposure affects basic brain architecture, while later exposure influences the fine-tuning of neural circuits. Disruptions during specific windows can have lasting consequences for cognitive abilities and behavioral tendencies.
Stress hormones during pregnancy also influence fetal brain development. High maternal cortisol levels can affect the developing stress response system, potentially creating children who are more reactive to stress throughout their lives. This demonstrates how environmental influences on the mother’s hormonal state can have intergenerational effects on behavior and mental health.
The concept of critical periods means that some hormonal influences during development cannot be reversed later in life. Unlike activational effects that come and go with changing hormone levels, organizational effects create permanent changes in brain structure that influence behavior across the entire lifespan. This is why early experiences have such profound and lasting impacts on development.
Connecting this to memory development in early childhood shows how hormonal influences interact with cognitive development to shape learning abilities and emotional responses during crucial developmental periods.
The Teenage Brain and Hormone Revolution
Puberty represents one of the most dramatic hormonal transformations in human development, creating widespread changes in brain function, behavior, and social relationships. Understanding these changes helps explain why adolescence is often characterized by increased risk-taking, emotional intensity, and social sensitivity.
The pubertal hormone surge affects brain regions at different rates, creating a temporary imbalance between emotional reactivity and cognitive control. The limbic system, which processes emotions and rewards, develops rapidly during early adolescence and becomes highly responsive to hormonal influences. Meanwhile, the prefrontal cortex, responsible for impulse control and long-term planning, continues developing well into the twenties.
This developmental mismatch explains many typical adolescent behaviors. Teenagers often experience emotions more intensely than adults and may struggle with impulse control, not because they lack intelligence or moral understanding, but because their brains are temporarily unbalanced during this transitional period.
Sleep patterns change dramatically during puberty due to hormonal influences on circadian rhythms. Melatonin production shifts to later in the evening, making it difficult for teenagers to fall asleep early. At the same time, they need more sleep than adults for optimal brain development. This biological shift often conflicts with school schedules and social expectations, creating chronic sleep deprivation that affects mood, cognition, and behavior.
Risk-taking behavior increases during adolescence partly due to hormonal changes in reward processing. Dopamine responses to novel and potentially rewarding experiences become heightened, making new experiences feel particularly exciting. This increased reward sensitivity can lead to both positive exploration and potentially dangerous behaviors, depending on available opportunities and social influences.
Social behavior becomes increasingly important during adolescence as sex hormones influence social cognition and peer relationships. Teenagers become more sensitive to social evaluation and more motivated to gain status and acceptance within their peer groups. These changes serve important developmental functions, helping adolescents establish independence from their families and form the social skills needed for adult relationships.
Adult Cycles and Aging
Hormonal influences continue throughout adult life through daily, monthly, and seasonal cycles that affect mood, behavior, and cognitive performance. Recognizing these patterns can help individuals optimize their daily routines and understand cyclical changes in their emotional and social experiences.
Daily cortisol rhythms influence energy levels, alertness, and stress resilience throughout the day. Most people show peak cortisol in the morning, which promotes wakefulness and prepares the body for daily challenges. This natural rhythm explains why many people feel most energetic and focused in the morning hours, with gradual decline in mental clarity and stress tolerance as the day progresses.
Monthly hormonal cycles in women create predictable changes in mood, social behavior, and cognitive abilities. The follicular phase (first half of cycle) often involves increased energy, sociability, and verbal abilities as estrogen rises. The luteal phase (second half of cycle) may bring increased introspection, emotional sensitivity, and preference for solitude as progesterone dominates. Understanding these patterns can help women plan important activities and social interactions to align with their natural rhythms.
Seasonal changes in daylight exposure affect melatonin and serotonin production, creating predictable mood and behavior changes throughout the year. Many people experience increased energy and sociability during longer summer days, while winter months may bring reduced motivation and increased desire for social withdrawal. These seasonal patterns vary by geographic location and individual sensitivity to light changes.
Table 3: Hormone Changes Across the Lifespan
| Life Stage | Key Hormones | Behavioral Changes | Adaptive Function |
|---|---|---|---|
| Prenatal | Testosterone, cortisol | Brain organization, stress sensitivity | Prepares for postnatal environment |
| Childhood | Growth hormone, cortisol | Learning, exploration, attachment | Supports development and learning |
| Puberty | Sex hormones, growth hormone | Risk-taking, social focus, identity formation | Prepares for adult roles |
| Young Adult | Peak sex hormones | Mate-seeking, competition, parenting | Reproductive success |
| Middle Age | Declining sex hormones | Increased wisdom, reduced risk-taking | Grandparenting, teaching |
| Older Adult | Low sex hormones, changed cortisol | Reduced aggression, increased cooperation | Social contribution, legacy |
Menopause and andropause (male menopause) create significant behavioral changes as sex hormone levels decline. Women often experience mood changes, altered sleep patterns, and shifts in social behavior during the menopausal transition. Men may notice reduced competitiveness, decreased risk-taking, and changes in emotional expression as testosterone gradually declines with age.
These hormonal changes associated with aging are not simply losses—they often represent adaptive shifts toward different life priorities. Reduced sex hormones may decrease competitive behaviors while enhancing cooperation and wisdom. Many older adults report increased emotional stability and life satisfaction, suggesting that hormonal changes can contribute to positive psychological development across the lifespan.
Mood, Mental Health, and Hormones
Depression and Anxiety Connections
The relationship between hormones and mental health conditions like depression and anxiety demonstrates the profound connections between biological systems and psychological well-being. Hormonal imbalances don’t cause mental health problems in isolation, but they significantly influence vulnerability, symptom severity, and treatment response.
Cortisol dysregulation appears in many forms of depression, particularly melancholic depression characterized by severe mood changes, sleep disturbances, and physical symptoms. Some depressed individuals show elevated cortisol levels throughout the day, while others have flattened daily rhythms that fail to provide the normal energy boost in the morning. These patterns often correlate with specific symptom profiles and treatment responses.
The HPA axis often becomes hyperactive during severe depression, creating a vicious cycle where stress hormones worsen mood symptoms, which in turn increase stress hormone production. This biological feedback loop helps explain why depression can be self-perpetuating and why effective treatments often need to address both psychological and biological aspects of the condition.
Thyroid hormones profoundly influence mood and cognitive function, with both hyperthyroidism (overactive thyroid) and hypothyroidism (underactive thyroid) creating psychiatric symptoms. Hypothyroidism often causes depression-like symptoms including fatigue, cognitive slowing, and mood changes, while hyperthyroidism can create anxiety, irritability, and racing thoughts. Thyroid screening is routine in mental health evaluations because hormone treatment can dramatically improve psychological symptoms.
Sex hormone fluctuations contribute to mood disorders in complex ways. Premenstrual dysphoric disorder (PMDD) involves severe mood changes related to normal cyclical hormone changes, demonstrating how normal biological processes can create significant psychological distress in sensitive individuals. Postpartum depression often coincides with dramatic hormonal changes after childbirth, though the relationship between hormone levels and mood symptoms is complex and mediated by multiple factors.
Anxiety disorders often involve dysregulated stress hormone systems that create heightened threat sensitivity and physical anxiety symptoms. People with panic disorder frequently show exaggerated cortisol responses to stress, while those with generalized anxiety may have chronically elevated baseline cortisol levels. Understanding these biological components helps explain why anxiety can feel overwhelming and why psychological interventions are often most effective when combined with attention to biological factors.
Seasonal Changes and Hormones
Seasonal Affective Disorder (SAD) demonstrates how environmental changes in light exposure can disrupt hormonal systems and create predictable mood changes. This condition provides a clear example of how external factors influence internal biological processes that determine behavior and emotional well-being.
Light exposure regulates melatonin production through direct connections between the eyes and the brain’s biological clock in the hypothalamus. During winter months with reduced daylight, melatonin production may begin earlier in the day and continue later into the morning, creating symptoms of fatigue, oversleeping, and depression-like mood changes.
Serotonin levels also fluctuate seasonally in response to light exposure, with many people showing reduced serotonin activity during dark winter months. Since serotonin influences mood, appetite, and social behavior, these seasonal changes can create significant shifts in psychological well-being and daily functioning.
The timing of sleep-wake cycles becomes disrupted when melatonin patterns shift, creating a cascade of effects on other hormonal systems. Cortisol rhythms may become flattened or delayed, affecting energy levels and stress resilience throughout the day. These multiple hormonal disruptions help explain why seasonal mood changes often involve complex combinations of sleep problems, appetite changes, and social withdrawal.
Light therapy works by resetting disrupted circadian rhythms and restoring normal hormonal patterns. Regular exposure to bright light in the morning helps maintain appropriate melatonin and cortisol rhythms, often providing significant relief from seasonal mood symptoms. This biological intervention demonstrates how understanding hormonal mechanisms can lead to effective, targeted treatments.
Understanding the connections between hormones and emotional regulation can be enhanced by learning about self-regulation in the early years, which shows how these systems develop and can be supported throughout life.
Modern Life and Hormonal Health
Technology and Hormone Disruption
Modern technology creates unprecedented challenges for hormonal systems that evolved over thousands of years in very different environments. Screen exposure, particularly blue light from electronic devices, can disrupt the natural production of melatonin and alter sleep-wake cycles in ways that cascade through other hormonal systems.
Blue light exposure in the evening suppresses melatonin production by signaling to your brain that it’s still daytime. This delay in melatonin release can shift your entire circadian rhythm, making it difficult to fall asleep at appropriate times and potentially affecting cortisol patterns the following day. The widespread use of smartphones, tablets, and computers in the hours before bedtime may be contributing to increased sleep problems and related mood changes in modern populations.
Social media use creates unique hormonal responses through its effects on social reward systems. The intermittent positive feedback from likes, comments, and social interactions can trigger dopamine release in patterns similar to gambling or other potentially addictive behaviors. While not involving traditional hormones, these neurotransmitter responses interact with hormonal systems and can influence mood, stress levels, and social behavior.
The constant connectivity enabled by modern technology may chronically activate stress response systems by making it difficult to fully disconnect from work or social pressures. The expectation of immediate responses to messages and the awareness of global events through 24-hour news cycles can maintain low-level stress activation that never allows hormonal systems to fully return to baseline levels.
Screen time also affects physical activity levels and outdoor light exposure, both of which influence hormonal health. Reduced physical activity can alter cortisol patterns, decrease natural mood-regulating hormones like endorphins, and affect sleep quality. Limited outdoor time reduces natural light exposure needed for healthy circadian rhythms and vitamin D production, which interacts with multiple hormonal systems.
Diet, Exercise, and Lifestyle Factors
Nutrition profoundly influences hormone production and signaling through direct effects on the building blocks needed for hormone synthesis and indirect effects on body weight, inflammation, and metabolic health. Understanding these connections helps explain how dietary choices can significantly impact mood, behavior, and cognitive performance.
Protein intake provides amino acids necessary for producing neurotransmitters and some hormones. Tryptophan, found in turkey and other foods, serves as a precursor for serotonin production and can influence mood and sleep quality. However, the relationship between dietary tryptophan and brain serotonin is complex, mediated by competition with other amino acids and influenced by carbohydrate intake.
Omega-3 fatty acids support healthy brain function and may help regulate inflammatory processes that interfere with normal hormone signaling. Regular consumption of fish, nuts, and other sources of healthy fats is associated with better mood regulation and may reduce the risk of depression. These effects likely occur through multiple mechanisms including direct effects on brain structure and indirect effects on inflammation.
Blood sugar stability affects multiple hormonal systems through its impact on insulin, cortisol, and other metabolic hormones. Large fluctuations in blood glucose can trigger cortisol release and create symptoms similar to anxiety or panic, while chronic high blood sugar can lead to insulin resistance that affects mood and cognitive function. Eating patterns that maintain stable blood sugar often improve emotional regulation and energy levels.
Exercise provides one of the most powerful tools for optimizing hormonal health through its effects on stress hormones, mood-regulating chemicals, and sleep quality. Regular physical activity helps regulate cortisol patterns, increases production of mood-enhancing endorphins, and improves sensitivity to insulin and other metabolic hormones.
Table 4: Lifestyle Factors and Hormone Health
| Factor | Hormone Impact | Behavioral Outcome | Optimization Strategy |
|---|---|---|---|
| Sleep Quality | Cortisol rhythm, melatonin | Mood stability, stress resilience | Consistent sleep schedule, dark environment |
| Physical Activity | Endorphins, cortisol, insulin | Enhanced mood, reduced anxiety | Regular moderate exercise |
| Nutrition | Serotonin, dopamine, cortisol | Stable mood, cognitive clarity | Balanced meals, stable blood sugar |
| Light Exposure | Melatonin, circadian rhythms | Sleep quality, seasonal mood | Morning sunlight, evening darkness |
| Social Connection | Oxytocin, cortisol | Stress resilience, emotional support | Quality relationships, community involvement |
| Stress Management | Cortisol, adrenaline | Emotional regulation, physical health | Mindfulness, relaxation techniques |
The timing of meals can influence circadian rhythms and hormonal patterns throughout the day. Eating large meals late in the evening can disrupt sleep and affect next-day cortisol patterns, while skipping breakfast may interfere with the natural morning cortisol rise that promotes alertness and energy. Meal timing that aligns with natural circadian rhythms often optimizes both metabolic and psychological well-being.
Alcohol and caffeine consumption significantly affect hormonal systems through their impacts on sleep quality, stress hormones, and neurotransmitter balance. While moderate caffeine intake can enhance alertness and mood, excessive consumption may increase anxiety and interfere with sleep. Alcohol may initially promote relaxation but often disrupts sleep architecture and can worsen mood and anxiety over time.
When to Seek Help: Clinical Applications
Recognizing Hormone-Related Issues
Understanding when behavioral or emotional changes might be related to hormonal issues can help individuals seek appropriate medical evaluation and treatment. While many hormonal fluctuations are normal and adaptive, certain patterns may indicate underlying health problems that benefit from professional intervention.
Sudden, dramatic changes in mood, energy, or behavior that cannot be explained by life circumstances may warrant hormonal evaluation. This is particularly true when changes persist for weeks or months despite attempts at lifestyle modifications or when they significantly interfere with work, relationships, or daily functioning.
Sleep disturbances that persist despite good sleep hygiene may indicate hormonal imbalances. Difficulty falling asleep, frequent nighttime awakening, or feeling unrefreshed despite adequate sleep time can all result from disrupted cortisol or melatonin patterns. When sleep problems coincide with mood changes, cognitive difficulties, or physical symptoms, hormonal evaluation may be helpful.
Physical symptoms that accompany behavioral changes often provide important clues about potential hormonal involvement. Unexplained weight changes, persistent fatigue, changes in appetite or digestion, temperature sensitivity, or changes in skin or hair quality may all reflect hormonal imbalances that are also affecting mood and behavior.
Cyclical patterns in symptoms can help identify hormone-related issues. Women who notice predictable changes in mood, energy, or cognitive function related to their menstrual cycles may benefit from evaluation for conditions like premenstrual dysphoric disorder or perimenopause. Men who experience gradual changes in energy, mood, or sexual function may be experiencing age-related testosterone decline.
Stress-related symptoms that seem disproportionate to life circumstances or that fail to improve with stress management techniques may indicate dysregulated stress hormone systems. This includes persistent anxiety, panic attacks, difficulty recovering from stressful events, or feeling “wired and tired” despite exhaustion.
Treatment Options and Support
Modern medicine offers various approaches to addressing hormone-related behavioral and emotional issues, ranging from lifestyle interventions to medical treatments. The most effective approaches typically combine multiple strategies tailored to individual needs and circumstances.
Hormone replacement therapy (HRT) can be beneficial for individuals with clinically low hormone levels, but it requires careful medical supervision and consideration of potential risks and benefits. Testosterone replacement may help men with clinically low levels who experience fatigue, mood changes, or cognitive difficulties. Estrogen replacement during menopause can alleviate mood changes, sleep disturbances, and cognitive symptoms, though individual risk factors must be carefully considered.
Lifestyle interventions often provide significant benefits for hormone-related issues and are typically recommended as first-line treatments or important adjuncts to medical therapy. Regular exercise, stress management techniques, improved sleep hygiene, and nutritional optimization can substantially improve hormonal balance and related behavioral symptoms.
Psychotherapy, particularly cognitive-behavioral therapy (CBT), can be highly effective for hormone-related mood and anxiety symptoms. CBT helps individuals develop coping strategies, challenge negative thought patterns, and make behavioral changes that support both psychological and hormonal health. The combination of therapy and medical treatment is often more effective than either approach alone.
Targeted supplements may help address specific nutritional factors that influence hormone production and signaling. Vitamin D, omega-3 fatty acids, magnesium, and B vitamins all play important roles in hormonal health, and deficiencies in these nutrients can contribute to mood and behavioral symptoms. However, supplement use should be guided by professional evaluation and monitoring.
Mind-body practices like meditation, yoga, and tai chi have demonstrated benefits for stress hormone regulation and overall well-being. These approaches work through multiple mechanisms including direct effects on the stress response system, improved sleep quality, and enhanced emotional regulation skills.
The connection between hormonal health and emotional regulation and building resilience in children shows how early interventions can support healthy development and prevent problems later in life.
Alternative and complementary approaches may provide additional support for hormonal health, though their effectiveness varies widely and scientific evidence is often limited. Acupuncture, herbal medicine, and other traditional healing approaches may benefit some individuals, but they should be used under professional guidance and in coordination with conventional medical care when appropriate.
It’s important to work with healthcare providers who understand the complex relationships between hormones, behavior, and mental health. Endocrinologists specialize in hormonal disorders, while psychiatrists and psychologists with knowledge of biological factors can provide integrated treatment approaches that address both psychological and physiological aspects of hormone-related issues.
Regular monitoring and follow-up are essential when treating hormone-related behavioral issues, as hormone levels and symptoms can change over time, and treatment approaches may need adjustment. What works well initially may become less effective, or changing life circumstances may require different therapeutic strategies.
The goal of treatment is not necessarily to achieve “perfect” hormone levels, but rather to optimize the balance between biological factors, psychological well-being, and quality of life. Many individuals find that understanding the hormonal components of their experiences helps them develop more effective coping strategies and make lifestyle choices that support their overall health and well-being.
Conclusion
Understanding the intricate connections between hormones and behavior reveals that we are neither purely products of our biology nor entirely in control of our responses. Instead, we exist in a dynamic interplay where chemical messengers shape our experiences while our choices and environment continuously influence these same systems.
The science of behavioral endocrinology demonstrates that hormones affect virtually every aspect of human experience—from the cortisol that helps you wake up each morning to the melatonin that prepares you for sleep each night. These chemical signals influence your stress responses, social relationships, cognitive abilities, and emotional regulation in ways that are both predictable and highly individual.
Most importantly, recognizing hormonal influences empowers you to make informed choices about your health and well-being. Whether optimizing your daily routines to support natural rhythms, seeking appropriate medical care when needed, or simply understanding why you feel different at various times, this knowledge provides valuable tools for navigating the complex relationship between your body and mind.
The field continues evolving as researchers discover new connections between hormonal systems and human behavior, promising even deeper insights into what makes us uniquely human while revealing the biological foundations we share with all living beings.
Frequently Asked Questions
What does the endocrine system do?
The endocrine system produces and releases hormones that regulate vital body functions including metabolism, growth, reproduction, mood, and stress responses. These chemical messengers travel through your bloodstream to target organs and tissues, coordinating complex physiological processes that keep you healthy and help you adapt to environmental changes.
How does the endocrine system influence behaviour?
Hormones directly affect brain regions controlling emotion, memory, and decision-making. Cortisol influences stress responses and memory formation, while sex hormones affect social behavior and aggression. These chemical signals create bidirectional relationships—your behaviors also influence hormone production, creating dynamic feedback loops throughout your day.
What are the 7 functions of the endocrine system?
The endocrine system regulates: (1) metabolism and energy balance, (2) growth and development, (3) reproduction and sexual function, (4) stress responses and adaptation, (5) sleep-wake cycles and circadian rhythms, (6) mood and emotional regulation, and (7) immune system function and inflammation responses.
What happens if your endocrine system is unhealthy?
An unhealthy endocrine system can cause mood disorders, sleep disturbances, unexplained weight changes, chronic fatigue, cognitive problems, and altered stress responses. Hormonal imbalances may lead to conditions like diabetes, thyroid disorders, depression, anxiety, and reproductive issues that significantly impact quality of life and daily functioning.
Which hormones most directly affect daily behavior?
Cortisol affects stress responses and energy levels, melatonin regulates sleep-wake cycles, serotonin influences mood and social behavior, dopamine drives motivation and reward-seeking, testosterone affects confidence and competition, and oxytocin enhances trust and social bonding. These hormones create observable changes in how you think, feel, and interact throughout each day.
Can lifestyle changes improve hormone-behavior relationships?
Yes, regular exercise, consistent sleep schedules, stress management techniques, balanced nutrition, and adequate sunlight exposure can significantly optimize hormonal balance. These lifestyle modifications often improve mood stability, stress resilience, cognitive performance, and emotional regulation by supporting natural hormonal rhythms and production.
When should I seek medical help for hormone-related behavior changes?
Consult healthcare providers if you experience persistent mood changes lasting several weeks, dramatic sleep disruptions despite good habits, stress responses disproportionate to situations, unexplained physical symptoms accompanying behavioral changes, or cyclical patterns that significantly interfere with work, relationships, or daily activities.
Do hormones affect men and women differently?
While both sexes share similar hormonal systems, sex hormones create different behavioral patterns. Women experience cyclical changes related to menstrual cycles, pregnancy, and menopause, while men show more stable but gradually declining hormone levels with age. However, individual variation within each sex often exceeds average differences between sexes.
References
Bauer, P. J. (2007). Remembering the times of our lives: Memory in infancy and beyond. Lawrence Erlbaum Associates.
Conkbayir, M. (2017). Emotional regulation in early childhood. Early Years Educator.
Department for Education. (2024). Statutory framework for the early years foundation stage. HM Government.
Donaldson, M. (1992). Human minds: An exploration. Allen Lane.
Eisenberg, N., Guthrie, I. K., Fabes, R. A., Shepard, S., Losoya, S., Murphy, B. C., Jones, S., Poulin, R., & Reiser, M. (1997). The relations of regulation and emotionality to resiliency and competent social functioning in elementary school children. Child Development, 68(2), 295-311.
Eisenberg, N., Spinrad, T. L., & Eggum, N. D. (2010). Emotion-related self-regulation and its relation to children’s maladjustment. Annual Review of Clinical Psychology, 6, 495-525.
Gathercole, S. E., & Pickering, S. J. (2000). Working memory deficits in children with learning difficulties. Academic Press.
Ghetti, S., & Bunge, S. A. (2012). Neural changes underlying the development of episodic memory during middle childhood. Developmental Cognitive Neuroscience, 2(4), 381-395.
Ginsburg, K. R., & Kinsman, S. B. (2014). Reaching teens: Strength-based communication strategies to build resilience and support healthy adolescent development. American Academy of Pediatrics.
Honig, A. S. (2002). Secure relationships: Nurturing infant/toddler attachment in early care settings. National Association for the Education of Young Children.
Lieberman, A. F. (2017). The emotional life of the toddler. Free Press.
Morelen, D., Shaffer, A., & Suveg, C. (2016). Maternal emotion regulation: Links to emotion parenting and child emotion regulation. Journal of Family Issues, 37(13), 1891-1916.
Morris, A. S., Silk, J. S., Steinberg, L., Myers, S. S., & Robinson, L. R. (2007). The role of the family context in the development of emotion regulation. Social Development, 16(2), 361-388.
Nelson, K. (2007). Young minds in social worlds: Experience, meaning, and memory. Harvard University Press.
Nutbrown, C. (2012). Foundations for quality: The independent review of early education and childcare qualifications. Department for Education.
Pascal, C., Bertram, T., Rouse, L., & Saunders, M. (2019). The reception baseline assessment research report. Department for Education.
Piaget, J. (1954). The construction of reality in the child. Basic Books.
Reframing Autism. (2023). Co-regulation and self-regulation. Reframing Autism.
Schore, A. N. (2015). Affect regulation and the origin of the self: The neurobiology of emotional development. Routledge.
Siraj-Blatchford, I., Sylva, K., Muttock, S., Gilden, R., & Bell, D. (2002). Researching effective pedagogy in the early years. Department for Education and Skills.
Tickell, C. (2011). The early years: Foundations for life, health and learning. Department for Education.
Whitebread, D. (2012). The importance of play. University of Cambridge.
Further Reading and Research
Recommended Articles
- Bauer, P. J. (2013). The development of forgetting: Childhood amnesia. In P. J. Bauer & R. Fivush (Eds.), The Wiley handbook on the development of children’s memory (pp. 519-544). John Wiley & Sons.
- Gunnar, M. R., & Quevedo, K. (2007). The neurobiology of stress and development. Annual Review of Psychology, 58, 145-173.
- Nelson, E. E., Leibenluft, E., McClure, E. B., & Pine, D. S. (2005). The social re-orientation of adolescence: A neuroscience perspective on the process and its relation to psychopathology. Psychological Medicine, 35(2), 163-174.
Suggested Books
- Sapolsky, R. M. (2017). Behave: The biology of humans at our best and worst. Penguin Press.
- Comprehensive examination of how biology, including hormones, influences human behavior across multiple timeframes from seconds to evolutionary history, with accessible explanations of complex neuroscience concepts.
- Brizendine, L. (2006). The female brain. Morgan Road Books.
- Explores how hormonal changes throughout women’s lives affect brain function, behavior, and emotional experiences from birth through menopause, with practical applications for understanding female development.
- Diamond, A., & Lee, K. (2011). Interventions shown to aid executive function development in children 4 to 12 years old. Science, 333(6045), 959-964.
- Evidence-based review of programs and activities that support the development of executive function skills, which are closely linked to hormonal and neurological maturation processes.
Recommended Websites
- Harvard Center on the Developing Child
- Comprehensive resource providing research-based information about early brain development, toxic stress, and the biological foundations of learning, behavior, and health across the lifespan.
- Society for Research in Child Development (SRCD)
- Professional organization offering research findings, policy briefs, and evidence-based resources on child development, including biological influences on behavior and learning.
- American Psychological Association (APA) – Developmental Psychology Division
- Access to current research, practice guidelines, and educational resources on developmental psychology, including hormonal influences on behavior across different life stages.
To cite this article please use:
Early Years TV The Endocrine System: Hormones and Behavior Connection. Available at: https://www.earlyyears.tv/the-endocrine-system-hormones-and-behavior-connection/ (Accessed: 26 February 2026).


